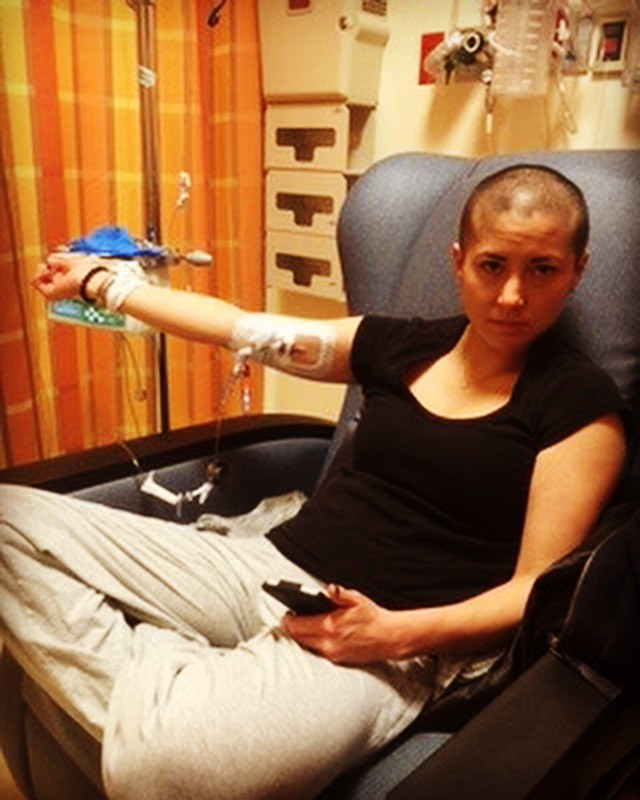
This is Casey Head and she is RESILIENT!

CONTENT WARNING: The I Am Resilient Project provides an open space for people to share their personal experiences. Some content in this post and on this website will include topics that you may find difficult.
Describe the situation where you had to be resilient:
I was in treatment for Acute Lymphoblastic Leukemia, then after four months, I had a stoke. It wasn’t part of the plan. Chemo along with the perfect storm of events caused me to have seizures and a stroke during cancer treatment. It left me temporarily paralyzed on my left side body. I had to relearn how to use my entire left side again from talking, walking to learning how to type all over again. I knew that if I ever wanted those things I would have to do the work required to make it happen, all while still undergoing chemo treatment. I realized early on in this process that if I could just learn how to tie my shoes myself that I would be okay. Somehow, I equated independence to putting on and tying my shoes by myself. That became my goal and focus. It was physically grueling and mentally exhausting for me. I was in rehab for my stroke for three hours every day for eight weeks, not missing one appointment. I showed myself that my body was way more resilient than I had ever thought possible.
Casey’s Story
Growing up I was always involved in sports, activities and playing outside until the street lights came on. I played three sports all through high school and went on to play two years of collegiate tennis. After graduating college in 2005, I moved back to Chicago. At 31 years old, my whole world changed. I was in the middle of a thriving career, newly married and trying to live life in Chicago.
Then my whole world came tumbling down when I was diagnosed with Acute Lymphoblastic Leukemia on 2/14/14. Happy valentine’s day to me. My initial symptom was a lump on my neck and I just assumed I was getting strep throat or something. I asked my husband if he had one and he said no. So, I set an appointment with an ENT (ear nose throat specialist). He felt it and said let’s try antibiotics and come back in two weeks. From the time I stopped taking the steroids, 5 days later I had my follow up appointment with the ENT. In those five days is when I really started to feel extreme fatigue. Huge bruises started showing up all over my body and by the morning of the appointment I was pale as a ghost and couldn’t make it up a flight of stairs without stopping to take a breath. I went to the ENT, my husband for some reason said he wanted to go with. I honestly thought what’s the big deal.
I saw the doctor and immediately he sent me across to another building to see an internist. He said I should go to the ER and get blood work done immediately because that would be the quickest way to get results. While I was waiting in the ER, that’s when they told me. That’s the moment my life changed forever. They said that they would have to confirm through biopsy but they were 99% sure it was cancer. That night as I was in an ambulance to downtown Northwestern Hospital in Chicago. I sat in the ER there waiting for a room to be ready. I told my husband that I couldn’t tell my dad, he had to. I couldn’t say the words. It wasn’t until years later that I could. Honestly, my husband took on the burden of telling friends, family and my work. I could not say the words.
I was immediately hospitalized for 28 days. Once it was confirmed through a bone marrow biopsy, or three to be exact, the doctor at the time thought he kept pulling cortical bone when my marrow was so impacted it just looked like bone, the medical team immediately started. Unfortunately, I was too sick to have fertility preservation done at that time. I only had 4 hemoglobin at the time and was immediately started on a two-year-long chemo protocol. I was able to get out a few days early because I promised to come back and lived only a few miles away from the hospital.
After leaving the hospital, I continued going to the doctors for infusions, treatments, test and everything else for 3-4 times a week. I was so grateful to be home but at the same time, it was exhausting going to the hospital that much for hours each time. Sometimes up to 10 hours with infusions, blood transfusions, platelet transfusions or vitamin infusions. I was exhausted physically but somehow keep going. I found out when I am in survivor mode, I handle most everything really well. My husband, dad and mother in law all come to every appointment (not all at the same time) but so I wouldn’t be alone or have to drive myself. My family had my back 100%. I felt like okay just take it day by day and do the best I could. I was somehow going to be the best patient I could be.
At the end of June 2014, I had a stroke from an unfortunate combination of a spinal tap with IT chemo that I had a CF leak from, dehydrated and didn’t eat for 3 days combined with peg asparaginase I had a stroke and seizures, a venous thrombosis. I went to the ICU and was placed into a medically induced coma.
The stroke left me temporarily paralyzed on my left side. I didn’t know at the time if I would ever be able to use my left side again. I felt numb. I couldn’t believe that I couldn’t use my left side. I literally felt and was helpless. No one would tell me if I was ever going to be able to use my left side either (you know they err on the side of caution) so it was very frustrating to figure out if I was going to be okay or not. After a stroke, you don’t think very clearly either so I was a bit out of it or like a zombie at times, maybe also because I was heavily medicated.
I was in the ICU for a few days until I could be sent to a rehabilitation hospital. I was there for about two weeks, over the Fourth of July weekend. At that point, I had to relearn how to walk, eat and move with my newly useless left side. This was probably one of my darkest moments. But I just knew that if I could somehow figure out how to tie my sneaker on my own that I would be okay. I just knew deep down inside somewhere that I could do it if I just keep working on it. If I just keep doing all the exercises eventually it’ll come back. I just didn’t know how long that would take but I wasn’t going to stop trying.
So that became my goal.
I spent the next 8 weeks going to rehab for three hours a day, five days a week. I never missed one session. Slowly, I regained the use of my left side. First working on my gait, movement of my left arm, and finally using my fingers, which proved to be the most difficult part. I had to relearn how to type, using the basic typing programs. All while still going through chemotherapy. My body was being pummeled in every way. I started going to gentle yoga through Gilda’s Club. Just knowing I wasn’t alone and seeing other survivors thrive regardless of diagnosis gave me more hope than anything else. There wasn’t anyone in particular but just being with a bunch of people that understood me without having to say anything was absolutely just transformative.
At the beginning of the end of October/early November 2016, I thought it would be good to go back to work. At this time, I was so desperate to get back to normal life. Seriously desperate. Looking back, I should not have gone back to work that soon. I wasn’t fully recovered from my stroke and still had yet to get into remission. My first remission came shortly after I went back to work, though. I thought I was on my way. I slowly started gaining weight, which turned into a lot of weight. I think I ended up putting on 20-30 ish pounds, the heaviest I had ever been. I was struggling to say the least.
So, I started to get more serious in my training. First with my own body weighted exercise and then picking up weights to get stronger. Shockingly no one said anything about the weight gain. I knew it was happening but I was in a bubble with people that knew what I was going through. I felt like a ball walking around all the time. Gross, disgusting and just since I was so fat, my hair was really short and I didn’t know what to do with it, my skin was discolored, I wasn’t sleeping I felt and looked like a mess. Like I didn’t have my sh*t together. I felt so uncomfortable in my own skin. I felt ugly. Mentally, due to the steroids, I became a crazy person. I had extreme mood swings. I was irritated and on edge all the time. I honestly did not feel like me. I was angry, frustrated and spiraling toward a negative wormhole. I sadly took all this out on my husband that bore the brunt of my frustration, I literally couldn’t help.
July 2015 is when I finally finished the chemotherapy for the ridiculous protocol, skipping the rest of the peg asparaginase, which I think was only three treatments left. Seven weeks later I relapsed. I thought I was doing well, starting to lose some of the weight and get back to normal. That was just the beginning.
Through blood work that I was still regularly getting checked, they found it early. I was immediately sent to the hospital. The doctors informed me that my cancer was not responding to chemotherapy the way they wanted. This is when I was started on my first of two immunotherapies’, Blinatumomab. The doctors concluded that chemo wasn’t working as effectively as they would like (basically, it wasn’t working). This is a 24 hour Fannie pack infusion system, I think about 3 days at a time before it gets changed. Well, I didn’t last that long. They sent me home and about 24 hours later went right back to the hospital. Spiking fevers of 105 degrees that the nurses on the cancer floor could not break. Close to being sent to the ICU, I managed to convince the intake doctor to let me stay. When the ICU doctor came back into the room, she said okay we’ll keep you here for now but if your temperature goes back up we’ll have to take you to the ICU. I said ok, I understand.
Now with chemo off the table and one immunotherapy out, I didn’t really have many options left. At the time Northwestern was working on a clinical trial, so we went down that path. I started to do all the testing required for the trial along with having my own stem cells harvested. That’s when we were told the trial was cancelled. There were two deaths from the trial and the drug company decided to pull it. It was a little more complicated but the abridged version will suffice for now. Basically, I didn’t have options.
The leukemia and lymphoma conference for doctors had just concluded and my medical team suggested that another immunotherapy may work. There wasn’t very much information and wasn’t intended for ALL refractor patients either. The only information we had to base our decision on was two pages of research of which 41 people participated and only 11 had acute lymphoblastic leukemia. I had no other options and the worst case would be to have me possibly transferred me to another hospital for a different clinical trial but was full at the time. So, I waited. I felt like I was watching my life on a TV screen. I was there but I wasn’t really there. It was dreamlike. I had to tell my dad that I didn’t know if I would live or die and his response was “well sometimes we don’t all make it to the end”. That moment I was really mad that he said it but now looking back I totally understand it. He himself was coping with that reality just as much as I was. My husband and I talked a lot about how I wanted him to keep living regardless of the outcome. My friends were just trying to keep it light around me, distract me. I had no idea how everyone else was feeling. I felt robbed and hopeful at the same time.
With over 60 days in the hospital, I was starting to go a little stir crazy, as you can imagine. But the doctors suggested I try the FLAG protocol of chemotherapy just in case it might work. It’ a combination of fludarabine, high dose cytarabine and filgrastim, normally for relapsed AML patients. Well, shocking it did not work. After 62 days, they sent me home in hopes that with a letter of compassion sent to Pfizer, which they approved and then one the FDA, for approval. I was released out of the hospital just before Christmas. I thought it was going to be my last one so I tried to soak in every moment I could. I then spent the next month and a half cleaning out closets, going to the gym and figuring out what my husband would need if I weren’t there. You know exactly the opposite of what you would think a person would do if they didn’t know if they were going to live or die.
I was finally approved for the immunotherapy, Inotuzumab which worked. I was in remission again. Headed straight into the hospital for a stem cell transplant. After more chemo and total body radiation, it was stem cell time. The anticipation was nerve-racking. I didn’t Google anything. I didn’t want to know what was about to happen. I didn’t ask, I only went by what the doctors were telling me. I was already mentally preparing for the worst possible outcome but hoping for anything but that. I was a bundle of anxiety. I was already feeling the effects of the chemo and rads which left me a little loopy high on all the meds but I was so worried it wasn’t going to work, deep inside.
My new birthday is on 2/21/17. Graft vs. host disease (GVHD) was now happening in full effect. It caused me to have mouth sores, strange rashes everywhere, bloating, constipation plus I couldn’t urinate and other such weird things happening. I did not feel at all like myself. I couldn’t pee for some reason so I was retaining all the liquids that I was ingesting. I started to have really intense panic attacks. I finally went home after 32 days in the hospital riddled with anxiety and retaining over 30 lbs of water. Trust me, I couldn’t even wear a bra because it was too tight so heavy with water retention. I felt like a bloated whale waddling around. A week after I went home the water weight was finally coming off. The doctors didn’t know if it was water weight or another issue, they basically after transplant play whack-a-mole with your side effects, just making sure you are alive. I was terrified anxiety-ridden and relieved that it was just water weight. But that’s also when I became dangerously close to 100lbs so I was drinking Ensure supplement drinks like water trying to get my weight back up.
Seven months later as I was recovering slowly from my stem cell transplant, I heard the one piece of news that I didn’t even want to hear ever again, “Your cancer is back.” I was rushed into the hospital to confirm it with another bone marrow biopsy. It was confirmed that I relapsed again, for the third time. I didn’t know in that moment how I was going to get through it.
My husband held me as I cried and said that I just didn’t know if I could do it all again, go through treatment mentally and physically. I really took a minute to figure out if it was the path I wanted to go down. I was so exhausted that I just didn’t know what would happen nor was in a state to even try at that point. I just took a second, dug deep and knew that I had to fight again. I was not going to let all of my family down by giving up now. My medical team decided it would be best to do another round of immunotherapy, instead of another injection of stem cells. Thankfully Inotuzumab did work and I have been in remission since the end of October 2017.
All through treatment, hospitalizations and stroke I continued to incorporate exercise into my daily routine, the best that I could. I started with walks every day, continuing to set goals for myself to walk a little further, faster each time. Then I incorporated body weighted exercises eventually leading into weights. I grew stronger every day and it helped with the side effects of chemotherapy. I am now living my full life. Having decided to not go back to the corporate world, I have made health and fitness my priority. I received my 200-hour yoga teaching certification along with my personal training certification. I am using these skills to help other women going through cancer thrive by living the best life they can while undergoing treatment and transitioning into their new normal life again. Showing and teaching them that they can get through treatment in a healthier way through movement.
How did you practice resilience when faced with this challenge?
I just dug deep within myself and decided that I was going to do anything and everything in my power that I was going to get through each and every obstacle. My why truly became that I did not want to disappoint my family around me by just giving up, that if I didn’t do everything I could then I was letting cancer win. My brother always says that even when I was little, if I got something in my head I find a way to make it happen.
Please share one piece of advice for people who are going through a similar challenge
Never give up or lose hope. Choose to wake up every single day and do your best by setting small goals for yourself. Sometimes not looking at the big picture helps focus on the small steps needed to get there.
Are you ready to share your story of RESILIENCE? You can do that HERE and thank you for being brave and sharing your journey.